23 August 2019
https://www.who.int/news-room/fact-sheets/detail/lead-poisoning-and-health
Key facts
- Lead is a cumulative toxicant that affects multiple body systems and is particularly harmful to young children.
- Lead in the body is distributed to the brain, liver, kidney and bones. It is stored in the teeth and bones, where it accumulates over time. Human exposure is usually assessed through the measurement of lead in blood.
- Lead in bone is released into blood during pregnancy and becomes a source of exposure to the developing fetus.
- There is no level of exposure to lead that is known to be without harmful effects.
- Lead exposure is preventable.
Lead is a naturally occurring toxic metal found in the Earth’s crust. Its widespread use has resulted in extensive environmental contamination, human exposure and significant public health problems in many parts of the world.
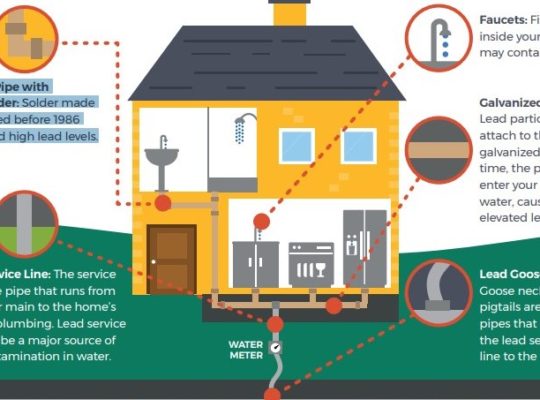
Important sources of environmental contamination include mining, smelting, manufacturing and recycling activities, and, in some countries, the continued use of leaded paint, leaded gasoline, and leaded aviation fuel. More than three quarters of global lead consumption is for the manufacture of lead-acid batteries for motor vehicles. Lead is, however, also used in many other products, for example pigments, paints, solder, stained glass, lead crystal glassware, ammunition, ceramic glazes, jewellery, toys and in some cosmetics and traditional medicines. Drinking water delivered through lead pipes or pipes joined with lead solder may contain lead. Much of the lead in global commerce is now obtained from recycling.
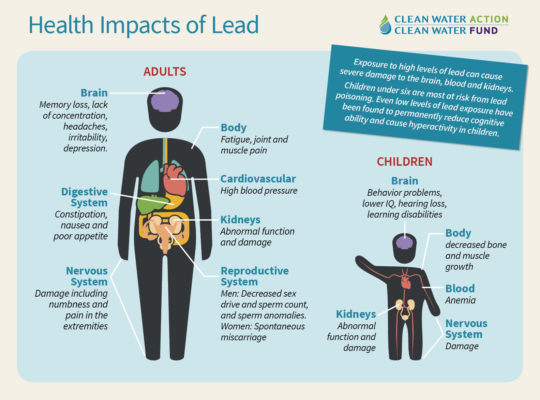
Young children are particularly vulnerable to the toxic effects of lead and can suffer profound and permanent adverse health effects, particularly affecting the development of the brain and nervous system. Lead also causes long-term harm in adults, including increased risk of high blood pressure and kidney damage. Exposure of pregnant women to high levels of lead can cause miscarriage, stillbirth, premature birth and low birth weight.
Sources and routes of exposure
People can become exposed to lead through occupational and environmental sources. This mainly results from:
- inhalation of lead particles generated by burning materials containing lead, for example, during smelting, recycling, stripping leaded paint, and using leaded gasoline or leaded aviation fuel; and
- ingestion of lead-contaminated dust, water (from leaded pipes), and food (from lead-glazed or lead-soldered containers).
An additional source of exposure is the use of certain types of unregulated cosmetics and medicines. High levels of lead have, for example, been reported in certain types of kohl, as well as in some traditional medicines used in countries such as India, Mexico and Viet Nam. Consumers should therefore take care only to buy and use regulated products.
Young children are particularly vulnerable to lead poisoning because they absorb 4–5 times as much ingested lead as adults from a given source. Moreover, children’s innate curiosity and their age-appropriate hand-to-mouth behaviour result in their mouthing and swallowing lead-containing or lead-coated objects, such as contaminated soil or dust and flakes from decaying lead-containing paint. This route of exposure is magnified in children with a psychological disorder called pica (persistent and compulsive cravings to eat non-food items), who may, for example pick away at, and eat, leaded paint from walls, door frames and furniture. Exposure to lead-contaminated soil and dust resulting from battery recycling and mining has caused mass lead poisoning and multiple deaths in young children in Nigeria, Senegal and other countries.
Once lead enters the body, it is distributed to organs such as the brain, kidneys, liver and bones. The body stores lead in the teeth and bones where it accumulates over time. Lead stored in bone may be remobilized into the blood during pregnancy, thus exposing the fetus. Undernourished children are more susceptible to lead because their bodies absorb more lead if other nutrients, such as calcium or iron, are lacking. Children at highest risk are the very young (including the developing fetus) and the economically disadvantaged.
Health effects of lead poisoning on children
Lead exposure can have serious consequences for the health of children. At high levels of exposure, lead attacks the brain and central nervous system to cause coma, convulsions and even death. Children who survive severe lead poisoning may be left with mental retardation and behavioural disorders. At lower levels of exposure that cause no obvious symptoms lead is now known to produce a spectrum of injury across multiple body systems. In particular lead can affect children’s brain development resulting in reduced intelligence quotient (IQ), behavioural changes such as reduced attention span and increased antisocial behavior, and reduced educational attainment. Lead exposure also causes anaemia, hypertension, renal impairment, immunotoxicity and toxicity to the reproductive organs. The neurological and behavioural effects of lead are believed to be irreversible.
There is no known ‘safe’ blood lead concentration; even blood lead concentrations as low as 5 µg/dL, may be associated with decreased intelligence in children, behavioral difficulties and learning problems. As lead exposure increases, the range and severity of symptoms and effects also increases.
Encouragingly, the successful phasing out of leaded gasoline in most countries, together with other lead control measures, has resulted in a significant decline in population-level blood lead concentrations. There is now only one country that continues to use leaded fuel (1). More, however, needs to be done regarding the phasing out of lead paint: so far only 37% of countries have introduced legally binding controls on lead paint (2)
Burden of disease from lead exposure
The Institute for Health Metrics and Evaluation (IHME) estimated that in 2017, lead exposure accounted for 1.06 million deaths and 24.4 million years of healthy life lost (disability-adjusted life years (DALYs)) worldwide due to long-term effects on health. The highest burden was in low- and middle-income countries. IHME also estimated that in 2016, lead exposure accounted for 63.2% of the global burden of idiopathic developmental intellectual disability, 10.3% of the global burden of hypertensive heart disease, 5.6% of the global burden of the ischaemic heart disease and 6.2% of the global burden of stroke (3).
WHO response
WHO has identified lead as 1 of 10 chemicals of major public health concern, needing action by Member States to protect the health of workers, children and women of reproductive age.
WHO has made available through its website a range of information on lead, including information for policy-makers, technical guidance and advocacy materials.
WHO is currently developing guidelines on the prevention and management of lead poisoning, which will provide policy-makers, public health authorities and health professionals with evidence-based guidance on the measures that they can take to protect the health of children and adults from lead exposure.
Since leaded paint is a continuing source of exposure in many countries, WHO has joined with the United Nations Environment Programme to form the Global Alliance to Eliminate Lead Paint. This is a cooperative initiative to focus and catalyse efforts to achieve international goals to prevent children’s exposure to lead from leaded paints and to minimize occupational exposures to such paint. Its broad objective is to promote a phase-out of the manufacture and sale of paints containing lead and eventually eliminate the risks that such paints pose.
The Global Alliance to Eliminate Lead Paint is an important means of contributing to the implementation of paragraph 57 of the “Plan of Implementation” of the World Summit on Sustainable Development and to resolution II/4B of the Strategic Approach to International Chemicals Management (SAICM), which both concern the phasing out of lead paint.
WHO is also a partner in a project funded by the Global Environment Facility that aims to support at least 40 countries in enacting legally binding controls on lead paint. (4)
The phasing out of lead paint by 2020 is one of the priority actions for governments included in the WHO Road map to enhance health sector engagement in the Strategic Approach to International Chemicals Management towards the 2020 goal and beyond. This road map was approved by the Seventieth World Health Assembly in decision WHA70(23).
The elimination of lead paint will contribute to the achievement of the following Sustainable Development Goal targets:
- 3.9: By 2030 substantially reduce the number of deaths and illnesses from hazardous chemicals and air, water, and soil pollution and contamination; and
- 12.4: By 2020, achieve the environmentally sound management of chemicals and all wastes throughout their life cycle, in accordance with agreed international frameworks, and significantly reduce their release to air, water and soil in order to minimize their adverse impacts on human health and the environment.
(1) Leaded Petrol Phase-out globally (2019)
Nairobi: United Nations Environment Programme; 2019.
(2) Global Health Observatory: Regulations and controls on lead paint.
Geneva: World Health Organization; 2019
(3) Institute for Health Metrics and Evaluation (IHME). GBD Compare.
Seattle, WA: IHME, University of Washington; 2017.
(4) SAICM GEF Project – Lead in Paint Component
https://www.who.int/news-room/fact-sheets/detail/lead-poisoning-and-health